PRIORITIES: Home-Based Palliative Care | Enhancing Competencies
eiCOMPASS PROJECT
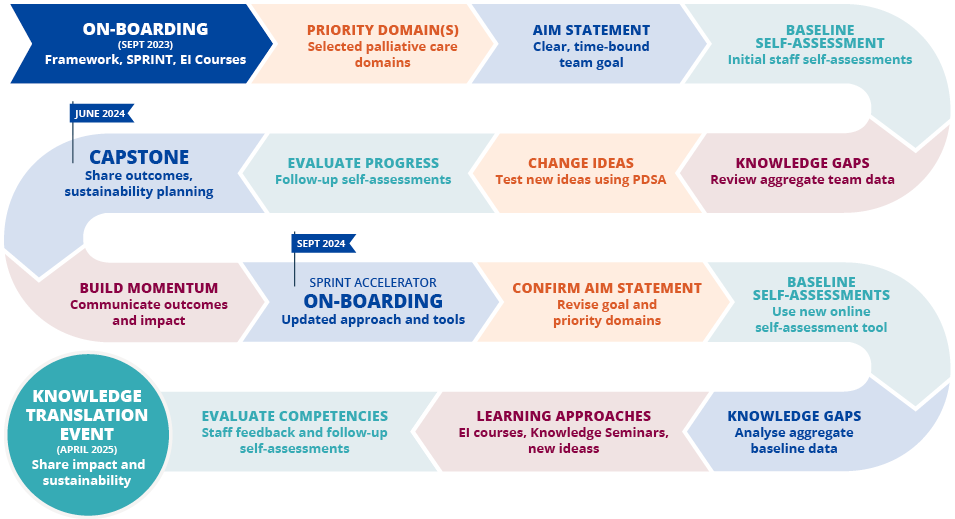
A core element of the eiCOMPASS Project is collaboration with home-based palliative care providers to facilitate the implementation of the Canadian Interdisciplinary Palliative Care Competency Framework, along with a suite of Emotional Intelligence (EI) online training programs and tools. We are achieving this objective through our SPRINT Implementation Collaborative.