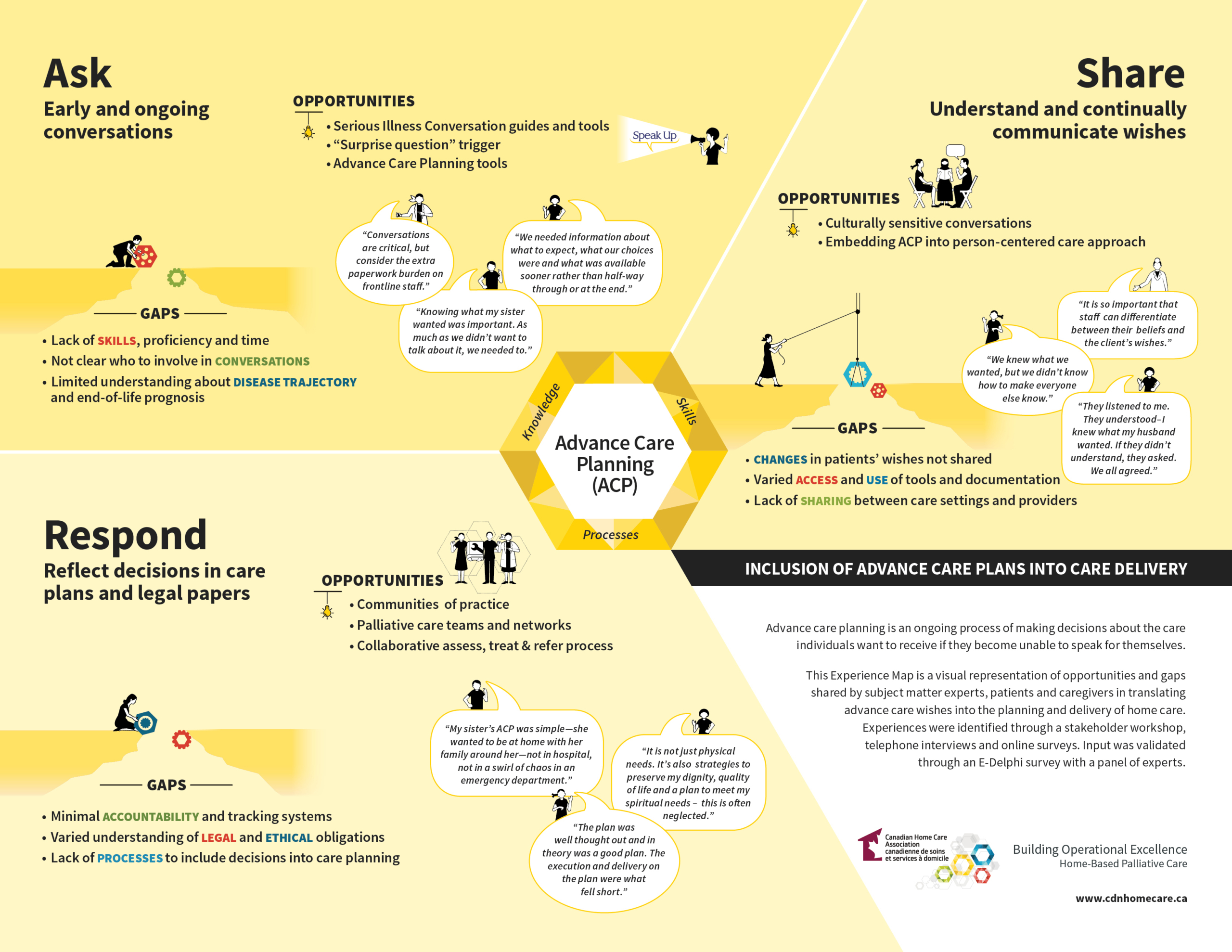
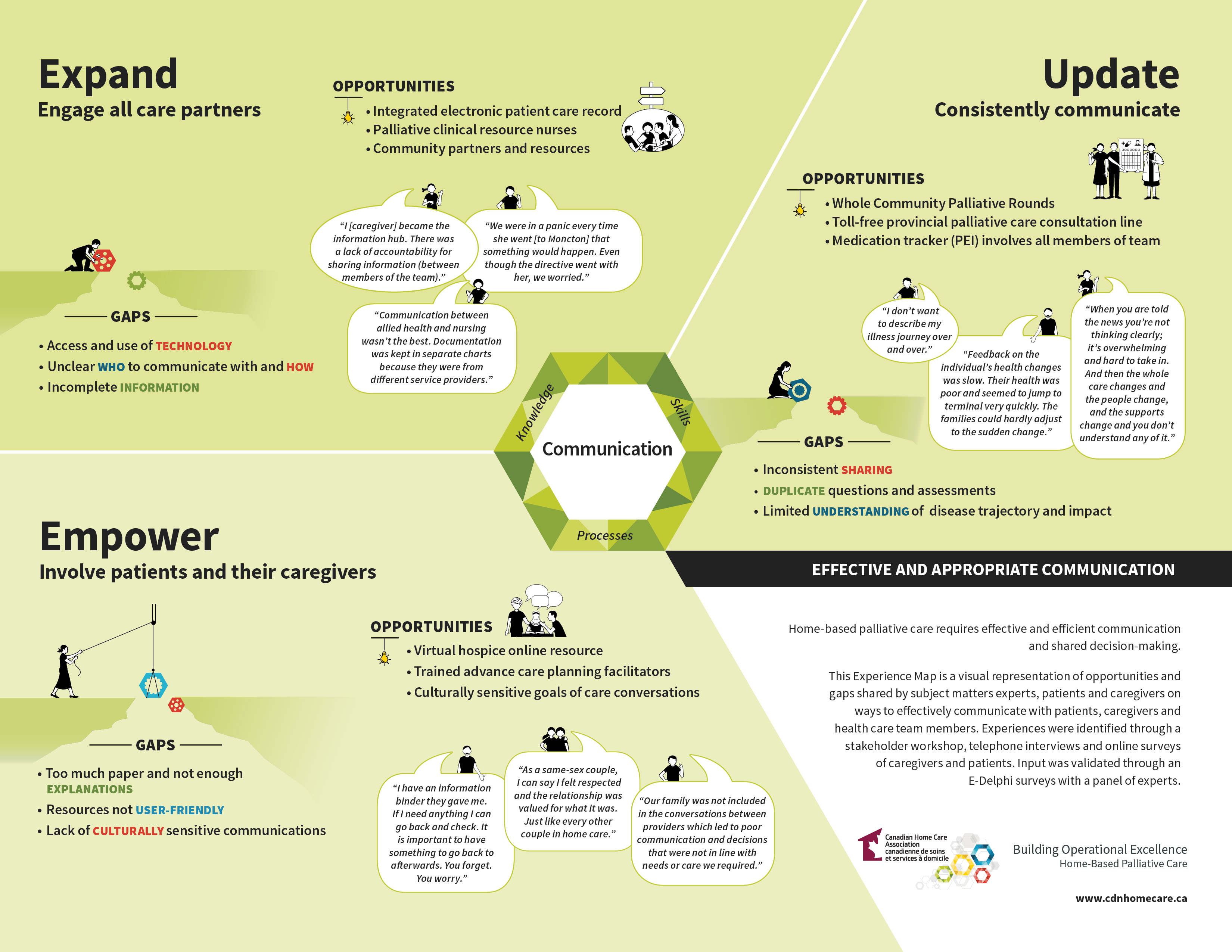
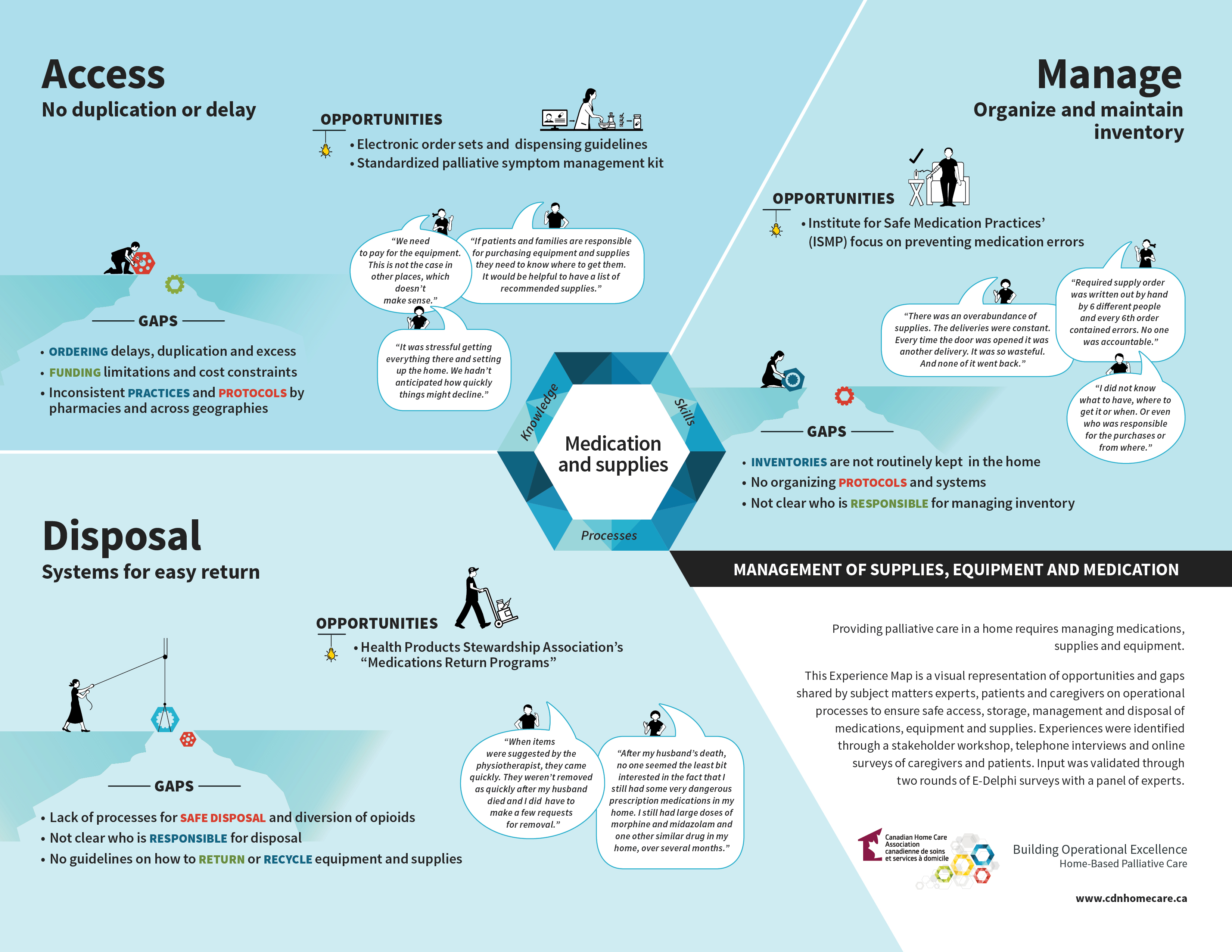
To better understand the realities of delivering and receiving home-based palliative care, the CHCA conducted an in-depth experience mapping process aimed at identifying barriers and opportunities from the perspectives of patients, caregivers, healthcare providers, funders and administrators. Through a multi-phased engagement approach that included regional workshops, key informant interviews, patient and caregiver surveys, and a national e-Delphi validation process, the CHCA received insights and experiences from more than 250 participants from across Canada.
Using an experience mapping process, the CHCA facilitated a structured and inclusive space for participants to reflect on how they think, feel, and act at key points along the palliative care journey. Discussions focused on four priority areas: advance care planning, assessment and care planning, communication, and the management of medications, equipment, and supplies.
The resulting experience maps offer both visual and narrative representations of the shared challenges and opportunities in home-based palliative care across the country. These insights are instrumental in shaping CHCA’s work on competency development.
Download the Summary Report : Mapping the Palliative Care Experience Multi-phase stakeholder engagement